Non-migrainous headaches often present with overlapping symptoms, making accurate diagnosis a significant challenge for healthcare professionals. Headaches are among the most common neurological complaints, yet not all are migraines. These types of headaches can stem from various causes such as tension, sinus issues, or cluster episodes, each requiring a distinct approach to treatment. Understanding their underlying mechanisms and differentiating them from migraine disorders is crucial for effective management.
In this article, we’ll explore the key diagnostic challenges, clinical evaluation methods, and evidence-based treatment strategies that help clinicians provide better patient outcomes. By highlighting the importance of early recognition and tailored care, this discussion aims to improve both headache management and patient quality of life.
Understanding Non-Migrainous Headaches
Definition and Overview
Non-migrainous headaches refer to a group of headache disorders that do not meet the diagnostic criteria for migraines. They encompass a wide range of conditions such as tension-type headaches, cluster headaches, sinus headaches, and secondary headaches resulting from medical or environmental factors. Unlike migraines, which are often throbbing and one-sided, non-migrainous headaches typically produce a steady, pressure-like pain that may affect both sides of the head. Understanding these distinctions is vital for clinicians, as misdiagnosis can lead to ineffective or inappropriate treatment.
Historical Background and Classification
The classification of headaches has evolved significantly over the years. The International Headache Society (IHS) developed detailed diagnostic criteria to help physicians differentiate between migraine and non-migraine types. Earlier, most headaches were broadly labeled as “tension headaches.” However, with advances in neurology and imaging techniques, experts now recognize multiple non-migrainous subtypes, each with its own triggers, symptoms, and treatment needs.
Common Types of Non-Migrainous Headaches
- Tension-Type Headache (TTH): Characterized by a dull, aching sensation with tightness around the scalp or neck. Often linked to stress, anxiety, or muscle tension.
- Cluster Headache: Intense, piercing pain around one eye or temple, often occurring in cyclical patterns or “clusters.”
- Sinus Headache: Associated with inflammation or congestion in the sinus cavities, leading to pressure in the forehead or cheekbones.
- Medication-Overuse Headache: Caused by frequent use of pain relief medications, leading to rebound headaches.
Importance of Accurate Diagnosis
Correct diagnosis is the cornerstone of effective headache management. Since non-migrainous headaches can mimic migraines or even coexist with them, a detailed patient history and clinical evaluation are essential. Misdiagnosis can result in overuse of migraine-specific medications, which may not alleviate symptoms. Instead, healthcare providers must focus on identifying triggers, lifestyle factors, and underlying health issues.
Key Diagnostic Tools
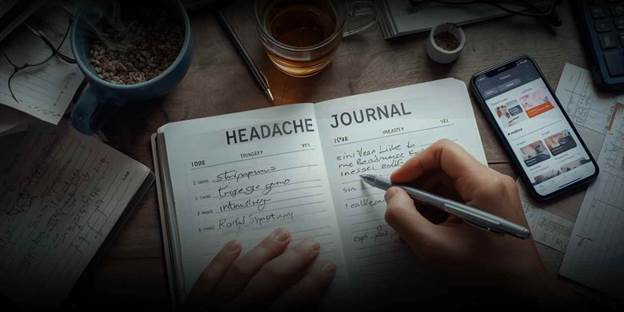
- Comprehensive patient history: Includes onset, duration, location, and pain characteristics.
- Physical examination: Assesses muscle tension, posture, and neck or shoulder tenderness.
- Imaging tests: MRI or CT scans help rule out serious causes like tumors or infections.
- Headache diaries: Encourage patients to track triggers, frequency, and response to medications.
Diagnostic Challenges
Diagnosing non-migrainous headaches can be complex due to overlapping symptoms with other headache disorders. For example, tension headaches may present with mild sensitivity to light or noise symptoms also seen in migraines. Furthermore, psychological stress, poor posture, and dehydration can blur diagnostic clarity.
Common Challenges Include:
- Difficulty distinguishing between primary and secondary headaches
- Variability of symptoms among patients
- Limited awareness of non-migraine headache patterns
- Overlapping triggers such as sleep deprivation and stress
Management and Treatment Strategies
1. Lifestyle Modifications
Lifestyle adjustments play a significant role in reducing headache frequency and severity. Encouraging healthy habits is often the first step in headache treatment.
Recommended approaches include:
- Maintaining regular sleep patterns
- Practicing relaxation techniques such as yoga or meditation
- Staying hydrated and avoiding excessive caffeine
- Reducing screen time and improving posture
- Incorporating daily physical activity
2. Pharmacological Approaches
While medication should be tailored to the type of headache, certain drugs provide relief across various non-migrainous types.
Common options include:
- Over-the-counter pain relievers such as acetaminophen or ibuprofen
- Muscle relaxants for tension-related pain
- Preventive medications like antidepressants or anticonvulsants in chronic cases
- Nasal decongestants for sinus-related headaches
It is crucial to avoid overusing pain medication, as it can lead to rebound headaches and dependency.
3. Physical and Behavioral Therapies
Non-drug therapies can be highly effective for tension-type headaches and other non-migrainous forms.
Examples include:
- Cognitive-behavioral therapy (CBT) to manage stress and anxiety
- Physical therapy to correct posture and relieve neck tension
- Biofeedback training to help patients gain control over muscle contractions
- Acupuncture and massage therapy for relaxation and pain relief
Preventive Care and Long-Term Benefits
Adopting preventive strategies can significantly enhance quality of life. Patients who learn to identify early warning signs can take proactive measures to prevent escalation. Regular follow-ups with healthcare providers ensure treatment plans remain effective and personalized.
Benefits of Effective Management:
- Reduced headache frequency and intensity
- Improved daily functioning and productivity
- Decreased reliance on pain medications
- Enhanced mental well-being
Real-Life Example
Consider a patient who experiences chronic neck and shoulder pain from prolonged computer use. Initially misdiagnosed with migraines, the individual later learns through clinical evaluation that they suffer from tension-type headaches. Through posture correction, ergonomic adjustments, and relaxation therapy, their symptoms dramatically decrease without the need for migraine-specific medication.
Future Perspectives
Ongoing research into headache neurobiology continues to refine our understanding of non-migrainous headaches. Advanced diagnostic imaging, genetic studies, and integrative treatment models are paving the way for more accurate diagnosis and individualized care. As awareness grows, healthcare professionals can expect to see better patient outcomes through early intervention and comprehensive management strategies.
Conclusion
Effective recognition and treatment of non-migrainous headaches are essential for improving patients’ daily functioning and long-term well-being. By understanding the different headache types, underlying causes, and appropriate management strategies, healthcare professionals can offer more accurate and lasting relief. Comprehensive diagnosis, lifestyle modifications, and preventive care play a vital role in successful headache management. As research advances, new approaches will continue to enhance treatment outcomes. To stay informed about the latest developments in headache treatment, explore updated clinical guidelines and emerging therapeutic options.